Our promise to you:
Guaranteed product quality, expert customer support.
 24x7 CUSTOMER SERVICE
24x7 CUSTOMER SERVICE
 CONTACT US TO ORDER
CONTACT US TO ORDER
Transfected Stable Cell Lines
Reliable | High-Performance | Wide Rage
Precision reporter, kinase, immune receptor, biosimilar, Cas9, and knockout stable cell lines for diverse applications.
Premade Virus Particles
Ready-to-Use | High Titer | Versatile Applications
Premade AAV, adenovirus, lentivirus particles, safe, stable, in stock.
Virus-Like Particles (VLPs)
Stable | Scalable | Customizable
Advanced VLPs for vaccine development (Chikungunya, Dengue, SARS-CoV-2), gene therapy (AAV1 & AAV9), and drug screening (SSTR2, CCR5).
Oligonucleotide Products
Precise | High Yield | Tailored Solutions
Accelerate your research with cost-effective LncRNA qPCR Array Technology.
RNA Interference Products
Targeted | Potent | High Specificity
Human Druggable Genome siRNA Library enables efficient drug target screening.
Recombinant Drug Target Proteins
Authentic | Versatile | Accelerated
Providing functional, high-purity recombinant proteins—including membrane proteins and nanodiscs—to overcome bottlenecks in drug screening and target validation.
Clones
Validated | Reliable | Comprehensive Collection
Ready-to-use clones for streamlined research and development.
Kits
Complete | Convenient | High Sensitivity
Chromogenic LAL Endotoxin Assay Kit ensures precise, FDA-compliant endotoxin quantification for biosafety testing.
Enzymes
Purified | Stable | Efficient
Powerful Tn5 Transposase for DNA insertion and random library construction.
Aptamers
Highly Specific | Robust | Versatile
Aptamers for key proteins like ACVR1A, Akt, EGFR, and VEGFR.
Adjuvants
Enhancing | Synergistic | Effective
Enhance immune responses with high-purity, potent CpG ODNs.
Laboratory Equipment
Innovative | Reliable | High-Precision
Effortlessly streamline DNA extraction with CB™ Magnetic-Nanoparticle Systems.
Stable Cell Line Generation
Reliable | Scalable | Customizable
Fast proposals, regular updates, and detailed reports; strict quality control, and contamination-free cells; knockout results in 4-6 weeks.
Target-based Drug Discovery Service
Innovative | Comprehensive | Efficient
Target identification, validation, and screening for drug discovery and therapeutic development.
Custom Viral Service
Versatile | High-Yield | Safe
Unbeatable pricing, fully customizable viral packaging services (covering 30,000+ human genes, 200+ mammals, 50+ protein tags).
Custom Antibody Service
Precise | Flexible | Efficient
End-to-end antibody development support, from target to validation, enabling clients to rapidly obtain application-ready antibodies.
Antibody-Drug Conjugation Service
Integrated | Controlled | Translational
Comprehensive solutions covering design, development, and validation to ensure conjugated drugs with consistent quality and clinical potential.
Protein Degrader Service
Efficient | High-Precision | Advanced Therapeutics
Harness the power of protein degraders for precise protein degradation, expanding druggable targets and enhancing therapeutic effectiveness for cutting-edge drug discovery.
Nucleotides Service
Accurate | Flexible | High-Quality
Custom synthesis of oligonucleotides, primers, and probes for gene editing, PCR, and RNA studies.
Custom RNA Service
Custom RNA ServicePrecise | Flexible | GMP-ReadyCustom
RNA design, synthesis, and manufacturing—covering mRNA, saRNA, circRNA, and RNAi. Fast turnaround, rigorous QC, and seamless transition from research to GMP production.
Custom Libraries Construction Service
Comprehensive | High-throughput | Accurate
Custom cDNA, genomic, and mutagenesis libraries for drug discovery, screening, and functional genomics.
Gene Editing Services
Precise | Efficient | Targeted
Gene editing solutions for gene editing, knockouts, knock-ins, and customized genetic modifications. Integrated multi-platform solutions for one-stop CRISPR sgRNA library synthesis and gene screening services
Microbe Genome Editing Service
Precise | Scalable | Customizable
Enhance microbial productivity with advanced genome editing using Rec-mediated recombination and CRISPR/Cas9 technologies.
Biosafety Testing Service
Reliable | Comprehensive | Regulated
Complete biosafety testing solutions for gene therapy, viral vectors, and biologics development.
Plant Genetic Modification Service
Advanced | Sustainable | Tailored
Genetic modification for crop improvement, biotechnology, and plant-based research solutions.
Plant-based Protein Production Service
Efficient | Scalable | Customizable
Plant-based protein expression systems for biopharmaceuticals, enzyme production, and research.
Aptamers Service
Innovative | Fast | Cost-Effective
Revolutionizing drug delivery and diagnostic development with next-generation high-throughput aptamer selection and synthesis technologies.
CGT Biosafety Testing
Comprehensive | Accurate | Regulatory-compliant
Internationally certified evaluation system for biologics, gene therapies, nucleic acid drugs, and vaccines.
Pandemic Detection Solutions
Rapid | Precise | Scalable
Balancing accuracy, accessibility, affordability, and rapid detection to safeguard public health and strengthen global response to infectious diseases.
cGMP Cell Line Development
Reliable | Scalable | Industry-leading
Stable expression over 15 generations with rapid cell line development in just 3 months.
Supports adherent and suspension cell lines, offering MCB, WCB, and PCB establishment.
GMP mRNA Production
Efficient | Scalable | Precise
Scalable mRNA production from milligrams to grams, with personalized process design for sequence optimization, cap selection, and nucleotide modifications, all in one service.
GMP Plasmid Production
High Quality | Scalable | Regulatory-compliant
Our plasmid production services span Non-GMP, GMP-Like, and GMP-Grade levels, with specialized options for linearized plasmids.
GMP Viral Vector Manufacturing
Scalable | High Yield | Quality-driven
Advanced platforms for AAV, adenovirus, lentivirus, and retrovirus production, with strict adherence to GMP guidelines and robust quality control.
AI-Driven Gene Editing and Therapy
Innovative | Precision | Transformative
AI-powered one-click design for customized CRISPR gene editing strategy development.
AI-Antibody Engineering Fusion
Next-Generation | Targeted | Efficient
AI and ML algorithms accelerate antibody screening and predict new structures, unlocking unprecedented possibilities in antibody engineering.
AI-Driven Enzyme Engineering
Smart | Efficient | Tailored
High-throughput enzyme activity testing with proprietary datasets and deep learning models for standardized and precise enzyme engineering design.
AI-Enhanced Small Molecule Screening
Predictive | Efficient | Insightful
Leverage AI to uncover hidden high-potential small molecules, prioritize leads intelligently, and reduce costly trial-and-error in early drug discovery.
AI-Driven Protein Degrader Drug Development
Innovative | Targeted | Accelerated
Use AI-guided design to optimize protein degraders, addressing design complexity and enhancing efficacy while shortening development timelines.



Cat.No. : CSC-RT2588
Host Cell: A549 Target Gene: EGFR
Size: 2x10^6 cells/vial, 1mL Validation: Sequencing
| Cat. No. | CSC-RT2588 |
| Description | This cell line is a stable cell line with a homozygous knockout of human EGFR using CRISPR/Cas9. |
| Target Gene | EGFR |
| Gene ID | 1956 |
| Genotype | EGFR (-/-) |
| Host Cell | A549 |
| Host Cell Species | Homo sapiens (Human) |
| Cell Type | Epithelial |
| Size | 2x10^6 cells/vial, 1mL |
| SequencingResult | 1 bp deletion in exon |
| Revival | Rapidly thaw cells in a 37°C water bath. Transfer contents into a tube containing pre-warmed media. Centrifuge cells and seed into a 25 cm2 flask containing pre-warmed media. |
| Media Type | Cells were cultured in DMEM/F12 supplemented with 10% fetal bovine serum. |
| Growth Properties | Cells are cultured as a monolayer at 37°C in a humidified atmosphere with 5% CO2. Split at 80-90% confluence, approximately 1:3-1:5. |
| Freeze Medium | Complete medium supplemented with 10% (v/v) DMSO |
| Mycoplasma | Negative |
| Format | One frozen vial containing millions of cells |
| Storage | Liquid nitrogen |
| Safety Considerations |
The following safety precautions should be observed. 1. Use pipette aids to prevent ingestion and keep aerosols down to a minimum. 2. No eating, drinking or smoking while handling the stable line. 3. Wash hands after handling the stable line and before leaving the lab. 4. Decontaminate work surface with disinfectant or 70% ethanol before and after working with stable cells. 5. All waste should be considered hazardous. 6. Dispose of all liquid waste after each experiment and treat with bleach. |
| Ship | Dry ice |
Cytotoxic T-lymphocyte antigen 4 (CTLA4) and programmed cell death protein 1 (PD-1) are immune checkpoint proteins expressed in T cells. Here, researchers found that CTLA4 is expressed in a subset of non-small cell lung cancer (NSCLC) cell lines and a subpopulation of cancer cells within lung cancer tissues. It was further found that in NSCLC cells, anti-CTLA4 antibodies can induce PD-L1 expression, which is mediated by CTLA4 and the EGFR pathway involving MEK and ERK phosphorylation. Anti-CTLA4 antibodies failed to induce PD-L1 expression in NSCLC cells in the presence of CTLA4 knockout cells, EGFR knockout cells, or in the presence of EGFR tyrosine kinase inhibitors. In addition, in the absence of adaptive immunity, anti-CTLA4 antibodies promoted NSCLC cell proliferation in vitro and tumor growth in vivo. These results suggest that tumor cell-intrinsic CTLA4 can regulate PD-L1 expression and cell proliferation, and that anti-CTLA4 antibodies, by binding to tumor cell-intrinsic CTLA4, may lead to activation of the EGFR pathway in cancer cells.
According to the study, both CTLA4 and PD-L1 are expressed at higher levels in EGFR wild-type or EGFR activating mutation NSCLC cells, and the researchers focused on determining the EGFR activation status. The study found that after anti-CTLA4 antibody treatment, phosphorylated EGFR (pEGFR) levels did increase in a dose-dependent manner, while total EGFR levels did not change (Figure 1A). On the other hand, IFN-γ treatment did not change pEGFR levels (Figure 1A). To further confirm this finding, the researchers examined the levels of phosphorylated MEK (pMEK) and phosphorylated ERK (pERK), downstream components of EGFR. The results showed that anti-CTLA4 also increased pMEK and pERK levels in a dose-dependent manner (Figure 1B). In contrast, IFN-γ increased the levels of phosphorylated S6 ribosomal protein (pS6) without changing the levels of pMEK and pERK (Figure 1B). In addition, the EFGR inhibitor canertinib suppressed pEGFR levels and also suppressed anti-CTLA4-induced PD-L1 expression levels (Figure 1C, lane 4). Notably, canertinib had no effect on IFN-γ-induced PD-L1 expression (Figure 1C, lane 3). In A549 EGFR knockout (KO) cells, anti-CTLA4 failed to induce PD-L1 expression (Figure 1D, lane 6), while IFN-γ-induced PD-L1 expression was intact (Figure 1D, lane 5). In A549 CTLA4 KO cells, anti-CTLA4-induced PD-L1 upregulation was also attenuated (Figure 1D, lane 9). Similarly, IFN-γ-induced PD-L1 expression was intact (Figure 1D, lane 8).
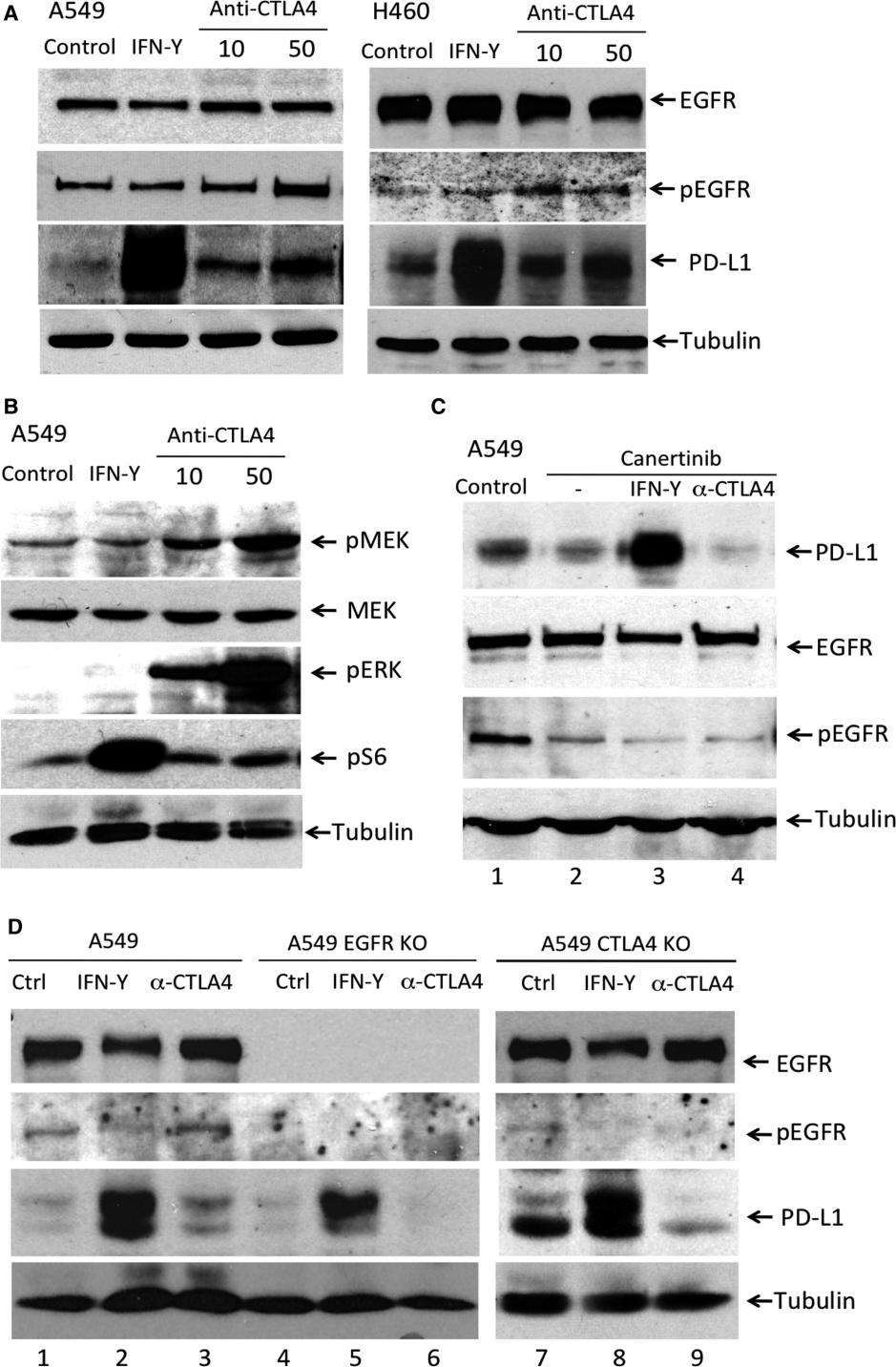 Figure 1. Anti-CTLA4 induced PD-L1 expression is EGFR pathway dependent in NSCLC cells. (Zhang H, et al., 2019)
Figure 1. Anti-CTLA4 induced PD-L1 expression is EGFR pathway dependent in NSCLC cells. (Zhang H, et al., 2019)
A: DMEM/F12 supplemented with 10% fetal bovine serum.
It is not required to add the selection antibiotics when culturing the KO cells.
A: The knockout cell product is validated by PCR amplification and Sanger Sequencing to confirm the mutation at the genomic level. Please find the detailed mutation info in the datasheet.
A: Single clonal cell.
A: No. This knockout cell product is generated using the CRISPR/Cas9 system to induce small insertions or deletions (indels) resulting in frameshift mutations. Although these frameshift mutations typically disrupt the coding gene, there is a possibility that the non-functional transcript may still be transcribed. Consequently, this could potentially yield misleading results when analyzed by RT-qPCR.
A: The cell line should be stored in liquid nitrogen for long-term preservation.
A: For most cases, we often keep at least 2 clones with different frameshift mutations. Please feel free to contact us to check if there are additional available clones.
If your question is not addressed through these resources, you can fill out the online form below and we will answer your question as soon as possible.
These EGFR knockout cells have been instrumental in advancing our understanding of EGFR signaling in cancer and its applications in cancer treatment.
United States
07/19/2022
Great buy! By using these cells as models of EGFR-dependent cancers, we can screen libraries of small molecules to identify potential inhibitors of EGFR signaling.
United States
11/03/2022
Write a review of your use of Biogene products and services in your research. Your review can help your fellow researchers make informed purchasing decisions.

Our promise to you:
Guaranteed product quality, expert customer support.
 24x7 CUSTOMER SERVICE
24x7 CUSTOMER SERVICE
 CONTACT US TO ORDER
CONTACT US TO ORDER

Copyright © Creative Biogene. All rights reserved.