What is mycoplasma?
Mycoplasma is the smallest known prokaryotic cell microorganism that can grow and reproduce on inanimate culture medium. It is divided into two genera: one is Mycoplasma, which has dozens of species; the other is Ureaplasma, which has only one species. Gram staining is negative, but not easy to stain. Generally, Giemsa staining is used to dye it light purple.
Mycoplasma is widely distributed in nature, has no cell wall, has a diameter of 0.1-0.3μm, and has a variable shape, and is very easy to pass through sterilization filters. Most mycoplasmas reproduce slower than bacteria, and the suitable growth temperature is 35℃. It is suitable for survival under alkaline conditions (pH7.6-8.0), has poor acid tolerance, and is sensitive to 75% ethanol and coal phenol soap solutions. If a lot of broken cells are found under the microscope during cell culture, and frequent changes of liquid are required to maintain subculture, mycoplasma contamination should be suspected. 95% of the mycoplasmas encountered in cell culture come from the following four types of mycoplasmas: oral mycoplasma, arginine mycoplasma, hyorhinal mycoplasma, and acholesterol mycoplasma, among which acholesterol mycoplasma is of bovine origin.
Effects of mycoplasma contamination
Mycoplasma contamination is a significant challenge in cell culture due to its often undetectable nature. Unlike easily identifiable bacterial contaminants that cause turbidity in culture media, mycoplasmas are cryptic pathogens. These parasitic bacteria act as metabolic competitors in the host cell environment. They compete for essential nutrients present in the culture medium, thereby impairing the growth and viability of cultured cells.
Mycoplasmas do not alter the pH or turbidity of the culture medium, but can affect changes in cell morphology, growth rate, metabolism, and function. Disruption of cellular homeostasis can lead to a range of deleterious effects, including:
- Cellular dysfunction: Mycoplasma contamination can alter gene expression and cell signaling pathways, ultimately leading to impaired cell function.
- Genomic instability: The presence of mycoplasmas can cause DNA damage and even chromosomal aberrations in host cells.
The consequences of mycoplasma contamination extend beyond the immediate loss of cell viability and compromised experimental data. Resources such as time, human effort, and financial investment invested in contaminated cultures are wasted. More importantly, studies based on mycoplasma-infected cells may produce inaccurate or misleading results, which may affect the validity of scientific publications and downstream applications, especially in biopharmaceutical production.
What causes mycoplasma contamination?
Mycoplasma contamination is a constant threat in cell culture because it is able to infiltrate cultures through a variety of routes. Here are the main culprits:
- Laboratory personnel: Surprisingly, humans are a significant contributor to mycoplasma contamination. Activities such as talking, coughing, or sneezing near cultures can generate aerosols that carry these microorganisms.
- Contaminated supplies: Mycoplasmas can lurk in a variety of cell culture supplies if not handled properly. This includes fetal bovine serum (FBS), cell culture media, and even incubator water baths if not sterilized regularly.
- Cross-contamination: This occurs when mycoplasmas are spread from infected cultures to uncontaminated cultures. Sharing pipettes or using multiple cell lines in close proximity increases this risk. Additionally, due to a lack of routine mycoplasma testing, some labs may receive contaminated cell lines without knowing it.
- External sources: Although less common, mycoplasmas occasionally enter the laboratory environment through external sources such as dust or airborne particles.
Detection and identification methods of mycoplasma contamination
- Isolation and culture method
The pathogen detection of mycoplasma is mainly determined by isolating and culturing mycoplasma from contaminated cells and chicken embryos. The isolation and culture method is the most reliable and accurate method for detecting mycoplasma contamination. However, mycoplasma is sensitive to environmental influences and is easily inactivated. Moreover, the isolation and culture operation is relatively cumbersome and takes a long time, so only qualitative observation of mycoplasma contamination can be performed. The isolation and culture method is often used to assist other detection methods in conventional mycoplasma detection.
- DNA fluorescence staining method
The DNA fluorescence staining method shortens the detection cycle compared to the isolation and culture method, and is mainly used for the detection of contaminated mycoplasma in cell culture. The DNA fluorescence staining method uses the principle that the fluorescent dye Bisbenzimidzole Hoechst33258 can bind to the A-T base-rich region in mycoplasma DNA. After staining, many uniformly sized fluorescent spots can be seen outside the nucleus and around the cells of cells contaminated with mycoplasma, which are mycoplasma DNA rich in A-T base regions.
- PCR technology
Specific primers are designed based on the conserved sequences in the mycoplasma genome to amplify the nucleic acid of the sample to be tested. The diagnosis is made by analyzing the size of the amplified product. PCR detection technology is used to detect mycoplasma contamination. It has a short cycle, high sensitivity, good specificity, simple operation, and can detect a large number of samples at one time.
- Enzyme-linked immunosorbent assay (ELISA)
ELISA is used to detect mycoplasma contamination. It has good specificity and sensitivity and can complete the detection of a large number of samples at one time.
Generally, after 48 to 72 hours of cell culture, before the cells are close to confluence, the cells are digested with trypsin to make a cell suspension, fixed, embedded, and sliced before observation.
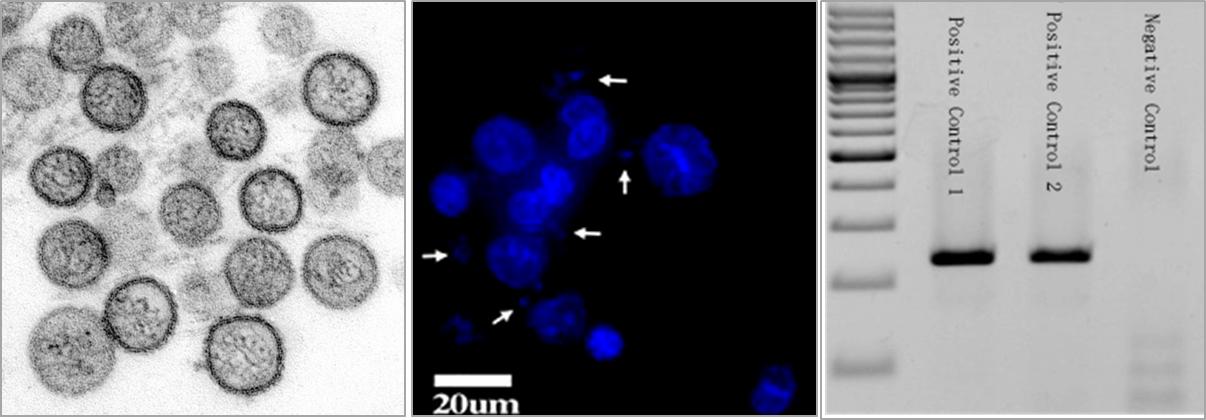
Figure 1. Various assays for mycoplasma testing.
How to prevent mycoplasma contamination in cell culture?
(1) Aseptic technique is essential
Maintaining a clean laboratory space is the most basic way to prevent contamination from occurring. When handling cell cultures, always prioritize aseptic technique. This includes washing hands frequently and using aseptic technique in all procedures. Regularly disinfect incubators, tissue culture hoods, and laboratory surfaces with appropriate disinfectants that are effective against mycoplasmas. Remember that mycoplasmas can ride on aerosols produced by talking or sneezing near cultures, so try to minimize talking in the cell culture hood.
(2) Minimize cross-contamination
Handling only one cell line at a time and having separate materials for each culture can help prevent the spread of mycoplasma. Do not reuse pipettes between cultures, and consider using dedicated equipment for handling cell lines with high flow rates.
(3) Routine screening: Eliminate mycoplasma before it causes damage
Regular monitoring of mycoplasma contamination is essential for early detection and prompt action. Many laboratories around the world neglect regular mycoplasma testing, and even with advanced detection methods, mycoplasma infection rates have remained virtually unchanged. The recommended interval for routine testing is 2 weeks to 3 months, depending on the cells you are growing in the lab.
| Cat.No. | Product Name | Price |
|---|---|---|
| BSK-01 | Mycoplasma Detection Kit | Inquiry |
| BSK-02 | Sample Prep Kit for Mycoplasma | Inquiry |
| PDPS-CN011 | Mycoplasma pneumoniae Real Time PCR Kit | Inquiry |
| PDPS-AR233 | Mycoplasma Genitalium (MG) Real Time PCR Kit | Inquiry |
| PDPS-AR234 | Mycoplasma Hominis (MH) Real Time PCR Kit | Inquiry |
| PDPS-AR053 | Mycoplasma Pneumoniae (MP) Real Time PCR Kit | Inquiry |
| PDPS-CN012 | Mycoplasma pneumoniae/Chlamydia pneumoniae Real Time PCR Kit | Inquiry |
| PDPS-CN029 | Mycoplasma hominis/Mycoplasma genitalium Real Time PCR Kit | Inquiry |
| PDPS-CN010 | Mycoplasma pneumoniae resistance mutation site Real Time PCR Kit | Inquiry |

