Most currently approved gene therapies, including those involving CRISPR-Cas9, involve gene editing of cells removed from the body outside the body and then infusing the edited cells back into the patient. This technology is ideal for targeting blood cells. Newly approved CRISPR gene therapies to treat blood diseases such as sickle cell anemia use this approach, in which gene-edited blood cells are reinfused into the patient after chemotherapy has destroyed the patient's bone marrow.
Now, in a new study, researchers from the University of California, Berkeley, have developed a new CRISPR-Cas9 precise targeted delivery method that can perform gene editing on very specific cell subpopulations in patients. It's a step toward programmable delivery methods that don't require destroying patients' bone marrow and immune systems before injecting them with gene-edited blood cells. The relevant research results were published in the journal Nature Biotechnology, and the paper is titled "In vivo human T cell engineering with enveloped delivery vehicles."
Jennifer Doudna, co-inventor of the CRISPR-Cas9 genome editing technology, developed the delivery method in her lab at the University of California, Berkeley. It encapsulates the Cas9 editing protein and guide RNA (gRNA) in a membrane vesicle decorated with monoclonal antibody fragments that target specific types of blood cells.
Jennifer Hamilton, a CRISPR researcher in Doudna's lab, demonstrated this by targeting the immune system's T cells, which are the starting point for a revolutionary cancer treatment called chimeric antigen receptor (CAR) T-cell therapy.
Hamilton and her colleagues treated live mice equipped with humanized immune systems to convert their human T cells into CAR T cells, allowing them to target and eliminate another type of immune cell called B cells. This feat is a proof-of-principle showing the potential of using this vector approach to envelope delivery tools to target and edit blood cells and possibly other cell types in living animals (in vivo), and ultimately in humans as well.
"Our approach involves multiplexing of targeting molecules, meaning we have two or more targeting molecules on our membrane vesicles," Hamilton said. "Their interaction with target cells is a bit like AND gates in computers, which are logic circuits that only work when two events occur at the same time."
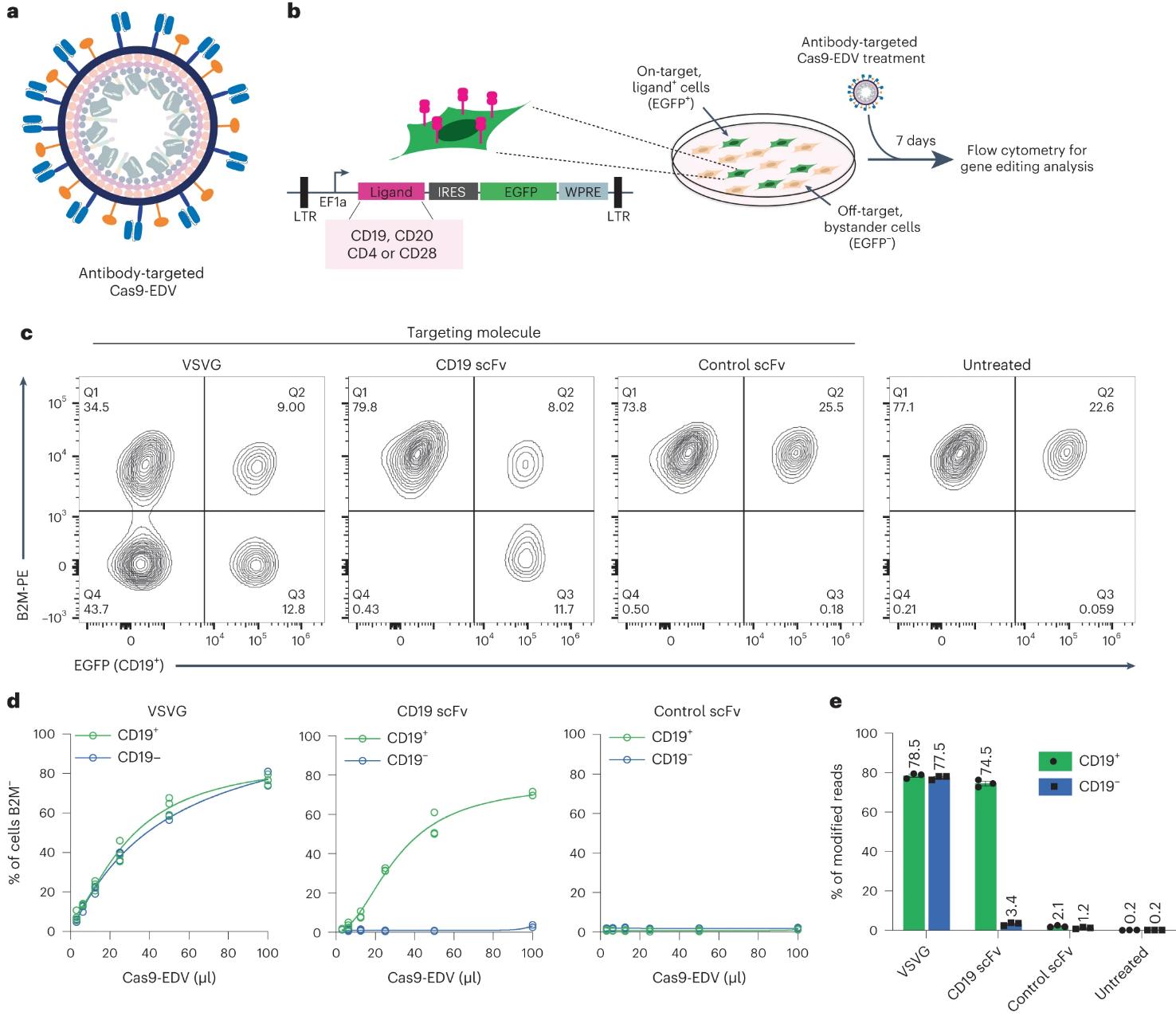
Figure 1. Cell-specific genome editing with antibody-targeted Cas9-EDVs. (Hamilton J R, et al., 2024)
"When membrane vesicles are bound using the interaction of two antibody ligands, we are able to achieve more efficient delivery. After treating mice with T cell-targeting vectors, we observed genome editing in the cell type of interest, T cells, but not hepatocytes," Hamilton said. "Highly specific targeting is difficult for all methods of delivering genes to cells. Liver cells, in particular, often take up delivery vehicles that are intended to be delivered elsewhere."
Hamilton and her team are working on one of several experimental techniques for delivering gene therapies. Many of these techniques use the shell of an enveloped virus—the virus is hollowed out and filled with corrective transgenes or gene-editing tools such as CRISPR-Cas9. Other approaches rely on injecting cell-penetrating Cas9 protein directly into mice to achieve genome editing. In a 2021 paper, she confirmed that after the outer envelope of the HIV-1 virus is hollowed out and filled with Cas9, T cells cultured in vitro can be edited and converted into CAR-T cells. Since then, she has made significant changes to viral envelopes and now calls them enveloped delivery vehicles (EDVs).
| CATALOG NO. | PRODUCT NAME | INQUIRY |
|---|---|---|
| CCP-001 | SpCas9 Nuclease | Inquiry |
| CCP-002 | SpCas9 Nuclease (+NLS) | Inquiry |
| CCP-003 | SpCas9 Nuclease (NLS) | Inquiry |
| CCP-004 | SpCas9 Nickase (D10A) | Inquiry |
| CCP-005 | SaCas9 nuclease | Inquiry |
| CCP-006 | AsCpf1 nuclease | Inquiry |
| CCP-007 | SpCas9-HF1 nuclease | Inquiry |
| CCP-008 | Anti-SpCas9 antibody | Inquiry |
| CCP-009 | Anti-SaCas9 antibody | Inquiry |
An important aspect of EDVs is that their outer envelope can be easily decorated with multiple antibody fragments or targeting ligands, thereby greatly improving targeting specificity. Other gene delivery vehicles, such as adeno-associated viruses and lipid nanoparticles, have proven more difficult to achieve precise targeting.
"People are trying to retarget all of these vectors to make them specific for one cell type and prevent gene delivery to other cell types," Hamilton said. "You can display antibodies or antibody fragments, as we have been doing, but the uptake rate by bystander cells is still high. You can favor delivery to one cell type, but you can still observe uptake by bystander cells. In our paper, we actually looked at the liver to see if there was anything off-target, and there wasn't. I think it's more challenging to achieve this with more traditional non-enveloped viral vectors or lipid nanoparticles."
In the paper, Hamilton and her colleagues sought to replicatein vivo a successful ex vivo CRISPR CAR-T cell therapy used in cancer patients. The therapy not only delivers a transgene encoding a receptor that targets cancer cells, but also uses CRISPR technology to knockout receptors that do not target cancer cells. They successfully knocked out the natural T-cell receptor and delivered a transgene encoding a receptor that targets B cells. Because the Cas9 protein is delivered in the same EDV as the transgene, it is shorter-lived than methods of delivering the Cas9 gene, meaning less off-target editing.
Reference
Hamilton J R, et al. In vivo human T cell engineering with enveloped delivery vehicles. Nature Biotechnology, 2024: 1-9.

