In clinical research, scientists have been looking for new ways to overcome type 1 diabetes. This disease plagues millions of patients worldwide. The patient's insulin-producing cells are mistakenly attacked by the immune system, causing blood sugar to soar, requiring lifelong dependence on insulin treatment.
However, recently, in a research report titled "Pharmacological inhibition of tyrosine protein-kinase 2 reduces islet inflammation and delays type 1 diabetes onset in mice" published in the international journal eBioMedicine, scientists from Indiana University School of Medicine and other institutions found through research that targeting an inflammation-related protein TYK2 may be expected to prevent or delay the progression of type 1 diabetes.
| Cat.No. | Product Name | Price |
|---|---|---|
| CLKO-0709 | TYK2 KO Cell Lysate-HEK293T | Inquiry |
| CSC-DC016910 | Panoply™ Human TYK2 Knockdown Stable Cell Line | Inquiry |
| CSC-RT0451 | TYK2 Knockout Cell Line-293T | Inquiry |
| CSC-SC016910 | Panoply™ Human TYK2 Over-expressing Stable Cell Line | Inquiry |
| AD17198Z | Human TYK2 adenoviral particles | Inquiry |
In recent years, the role of inflammation in type 1 diabetes has gradually become a research hotspot. The inflammatory response plays a key role in the development of type 1 diabetes. It not only destroys insulin-producing beta cells, but also intensifies the immune system's attack on these cells. Scientists have been looking for ways to precisely regulate inflammatory signaling pathways to protect beta cells from damage. As a key molecule in inflammatory signaling, the TYK2 protein has become a research focus. Previous research results have shown that people with lower TYK2 activity have a lower risk of type 1 diabetes, which provides a theoretical basis for therapeutic strategies targeting TYK2.
In this study, researchers used human cells and mouse models to explore the effects of TYK2 inhibitors on type 1 diabetes. They found that blocking the inflammatory signaling of TYK2 protein through molecular methods not only reduced harmful inflammation in the pancreas, but also protected beta cells from attacks by the immune system. The dual effects of this strategy are remarkable. On the one hand, it can directly protect insulin-producing cells, and on the other hand, it can indirectly reduce the damage of these cells by the immune system by inhibiting the inflammatory response.
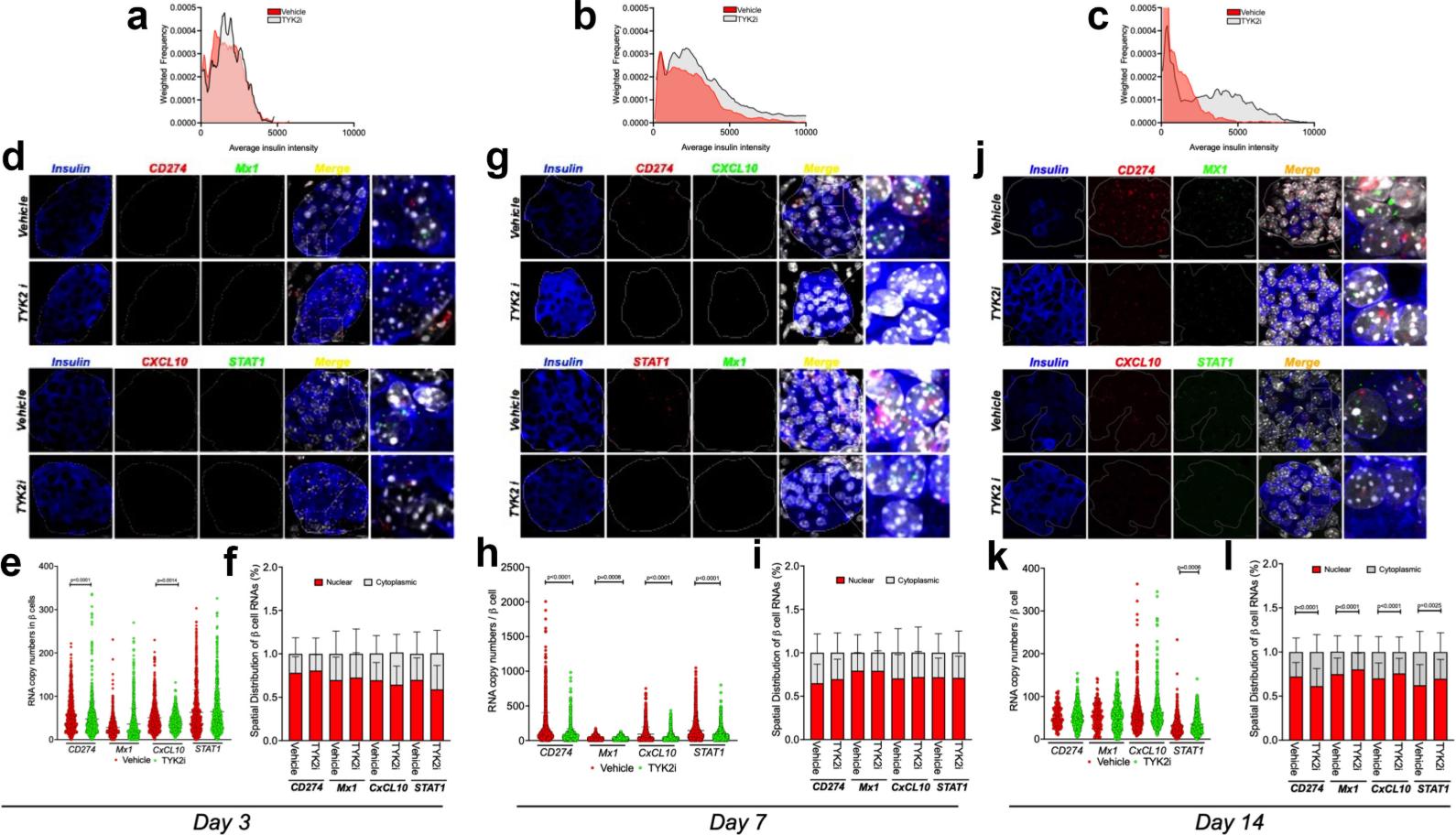
Figure 1. TYK2i treatment preserves pancreatic β cells and inhibits the expression of IFNα-induced mRNAs in RIP-LCMV-GP mice. (Syed F, et al., 2024)
This study not only reveals the important role of TYK2 in type 1 diabetes, but also provides a scientific basis for the reuse of an approved drug. At present, a TYK2 inhibitor for the treatment of psoriasis has been approved by the FDA. This means that the safety and effectiveness of this drug have been verified in the clinic, and its application in the translational research of type 1 diabetes treatment may be faster and smoother. Researcher Carmella Evans-Molina, PhD, said that targeting TYK2 may be a powerful method that can protect insulin-producing beta cells while alleviating the inflammatory response of the immune system at the same time. This discovery is exciting because there is already a drug on the market for psoriasis that can do this, which may help us advance clinical trials of type 1 diabetes faster.
In the article, the researchers first tested the effect of TYK2 inhibitors in human beta cells and dispersed adult islets. The results showed that this inhibitor can significantly reduce the beta cell inflammatory response induced by interferon α (IFNα), including reducing the overexpression of HLA class I molecules, reducing endoplasmic reticulum stress and the production of chemokines. In co-culture experiments with T cells, beta cells pre-treated with TYK2 inhibitors were able to prevent IFNα-induced T cell activation, thereby reducing the attack on insulin.
In mouse models, the researchers used two type 1 diabetes models (RIP-LCMV-GP mice and NOD mice) to evaluate the effects of TYK2 inhibitors. The results showed that this inhibitor can reduce systemic and local tissue inflammation to prevent beta cell death and delay the onset of type 1 diabetes. Using single-molecule fluorescence in situ hybridization (smFISH) technology, the researchers also found that TYK2 inhibitors can significantly reduce IFNα-induced mRNA expression in pancreatic islets, including genes such as PD-L1, CXCL10, STAT1 and MX1, whose expression is closely related to inflammatory response. The results of this study provide new ideas for the future treatment of type 1 diabetes. The researchers plan to conduct translational studies to evaluate the effects of TYK2 inhibitors alone or in combination with other approved drugs, especially in individuals at high risk or in the new stage of type 1 diabetes. If these studies can achieve positive results, TYK2 inhibitors are expected to become a new option for the treatment of type 1 diabetes.
The researchers pointed out that preclinical model studies have shown that this treatment method may also be effective in humans. The next step is to launch translational research to evaluate the effects of TYK2 inhibitors alone or in combination with other approved drugs in patients at high risk or newly diagnosed with type 1 diabetes. In summary, this groundbreaking study not only reveals the important role of TYK2 in type 1 diabetes, but also provides a scientific basis for the reuse of an approved drug. With more research, TYK2 inhibitors are expected to bring new hope to patients with type 1 diabetes and improve their quality of life.
Reference
Syed F, et al. Pharmacological inhibition of tyrosine protein-kinase 2 reduces islet inflammation and delays type 1 diabetes onset in mice. EBioMedicine, 2024.

