• Adenovirus Service • AAV Service • Lentivirus Service • Retrovirus Service


T cells are an important part of the body's immune system, helping not only to clear invading pathogens, such as viruses, but also to kill cancer cells.

Lung cancer is still the most common and deadly cancer in the world. Small cell lung cancer (SCLC) is the deadliest type of lung cancer, accounting for about 15% of all lung cancer cases. SCLC is an aggressive high-grade neuroendocrine tumor characterized by short doubling time, rapid growth, and early metastasis and spread. Most SCLC patients develop resistance rapidly, and their 5-year survival rate is very low (5-6%), even when the initial response to standard chemotherapy is good. The addition of immune checkpoint inhibitors to conventional chemotherapy for small cell lung cancer is promising; however, their absolute long-term benefits are moderate. The complex mechanisms of widespread SCLC metastasis and recurrence need to be clarified to expand the long-lasting benefits of chemotherapy and immunotherapy to more patients.

In the body, there are thousands of cells mutated due to DNA errors lurking every day, and they all have the possibility of eventually causing cancer. Existing theories believe that cancer is caused by two types of gene mutations: mutations of proto-oncogenes and inactivation of tumor suppressor genes, however, not all genetic mutations cause cancer. Take the mole on the body as an example, gene mutations can cause the mole to become cancerous and form melanoma. It is worth noting that most moles will never become cancerous. Scientists have been working to unravel the reasons for this difference, and this problem has finally been overcome recently.
In a new study, researchers from the University of Texas Southwestern Medical Center discovered an Achilles’ heel of ovarian cancer and new biomarkers that may indicate which patients are the best candidates for potential new therapies. Related research results are published online in the Cell journal.

Recently, at the 2021 American Society of Clinical Oncology (ASCO) annual meeting, researchers from the University of Sydney, Australia will announce the results of its RELATIVITY-047 trial. In this clinical trial, researchers discovered a new type of immune checkpoint Inhibitor that may effectively help save the lives of patients with malignant melanoma, and this breakthrough study may be extended to other cancer types.
Regulatory T (Treg) cells expressing CD4 and Foxp3 are the main regulators of autoimmune diseases. However, the temporal and spatial characteristics of tissue-specific autoimmune suppression mediated by Treg cells have not yet been clearly revealed. In a study recently published in the journal PNAS, Benoît L. Salomon's team from Sorbonne University in France further revealed the role of tumor necrosis factor receptor 2 (TNFR2) signaling in Treg cells during multiple sclerosis (EAE).
One of the main signs of chronic pain is inflammation. Recently, in a research report published in the international journal of Neuron, scientists from the University of North Carolina School of Medicine and other institutions have discovered through research that anti-inflammatory cells called MRC1+ macrophages may be dysfunctional in a mouse model of neuropathic pain. Promoting these cells to return to their normal state may be expected to help treat body pain caused by nerve damage or nervous system dysfunction. Researchers have shown that stimulating the expression of an anti-inflammatory protein called CD163 may reduce signs of neuroinflammation in the spinal cord of mice with neuropathic pain.
In previous studies, scientists have discovered that a protein called IL-24 attacks various cancers in many different ways. In a new study, through T cell engineering, researchers from Virginia Commonwealth University found that using T cells to deliver the gene encoding IL-24 (called MDA-7) to solid tumors can prevent tumor growth in a variety of cancers and inhibit the spread of cancer to other tissues. Relevant research results were published in the journal of Cancer Research.

The body’s immune response is a balanced behavior. Excessive amounts can lead to inflammation or autoimmune diseases. Too little can lead to serious infections. Regulatory T cells, or Tregs, are important to maintain this balance. It plays a role of "brake" in the immune response process of the body to avoid excessive immune response. Therefore, controlling the number and activity of Tregs is particularly important for maintaining the health of the body. Recently, in a research report published in the international Journal of Clinical Investigation, scientists from the University of Pennsylvania and other institutions have found that the molecule named DEL-1 can be used as an effective method to help treat inflammation or suppress autoimmune response by targeting. DEL-1 molecule can promote the production of Tregs and its immunosuppressive activity.

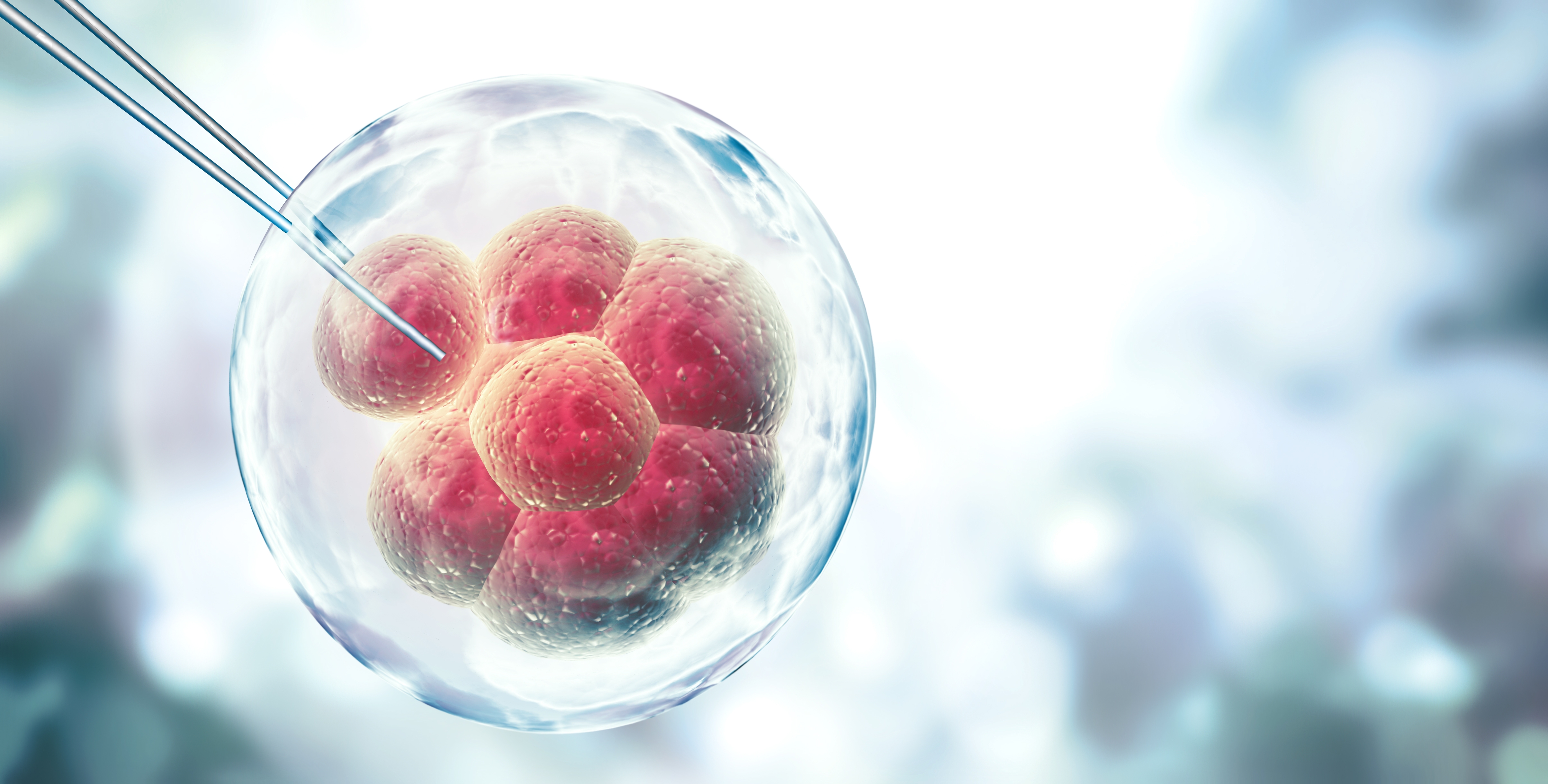
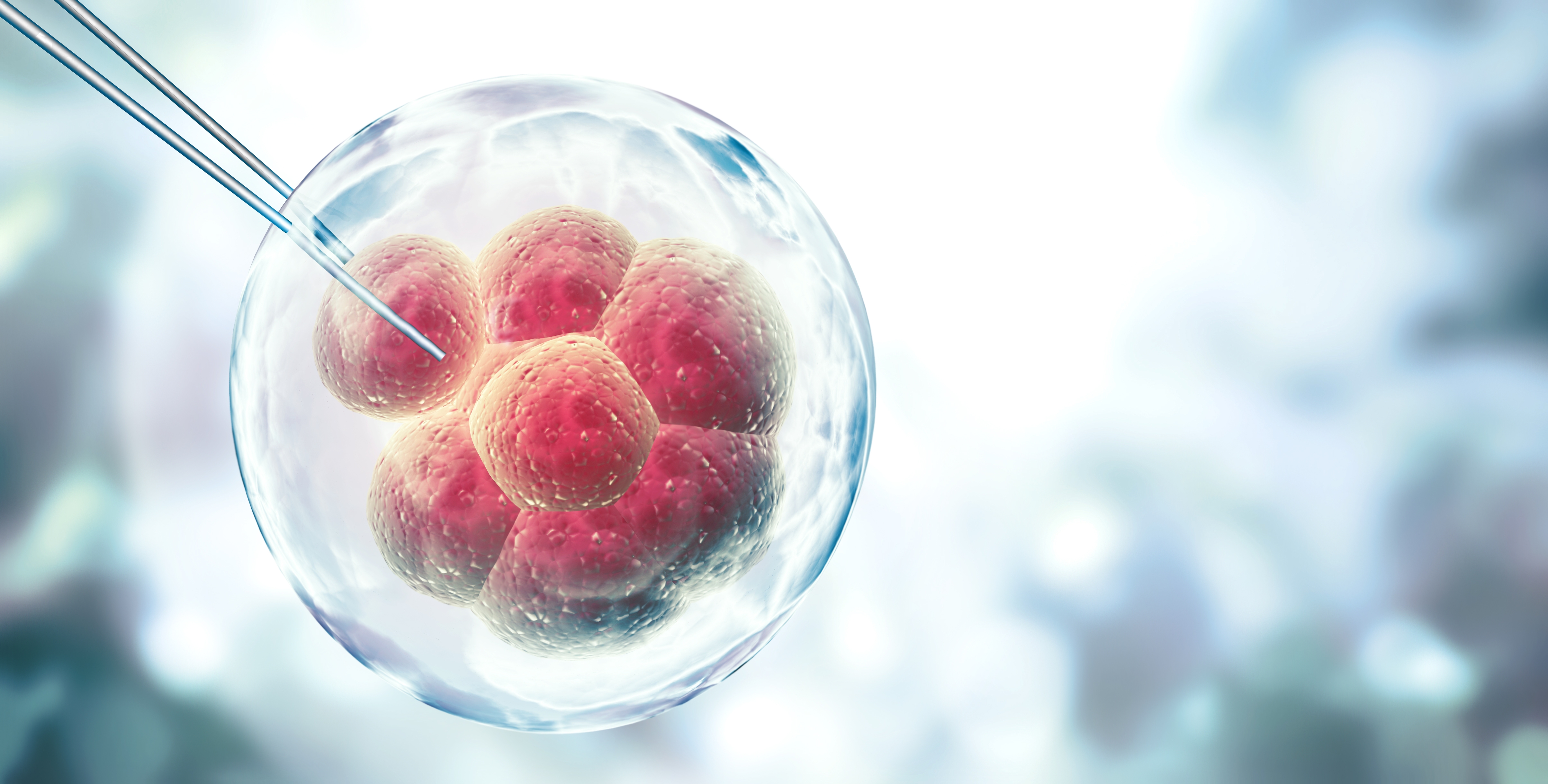
Recently, in a research report published in the international journal Proceedings of the National Academy of Sciences, scientists from the University of Alabama at Birmingham and other institutions have clarified the cause and molecular mechanism of the serious birth defect called CHARGE syndrome (CHARGE joint deformity, nostril atresia deformity) through research. In the article, the researchers successfully inactivated the CHD7 gene in mouse embryonic neural crest cells, and then tracked how the inactivation of the CHD7 gene in the developing cardiac neural crest cells induced serious defects in the right ventricular outflow tract and large arteries of the heart, and lead to perinatal death of the fetus. Heart defects and other birth defects in embryos are similar to human CHARGE syndrome defects. Currently, known CHD7 mutations can induce approximately 70% of human CHARGE syndrome.